What is Eczema or Atopic Dermatitis?
The words ‘dermatitis’ and ‘eczema’ mean the same thing. The word ‘atopic’ means ‘out of place’. It is a word used to describe a group of conditions which include eczema, asthma and hay fever.
Atopy, is where the body’s immune system overreacts to things that would not normally do any harm – often environmental factors that are all around us. For many children, especially those with more severe atopic dermatitis, the skin is also affected by genetic changes.
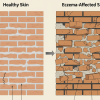
All children with eczema have dry skin, which allows entry to triggers – irritants (e.g. soaps, fragrance, detergents) and allergens (e.g. animal dander, house dust mite droppings and pollens) – which make their skin inflamed and itchy.

What is it like to have childhood atopic eczema?
Atopic eczema is a complex inflammatory skin condition. Children with eczema have dry skin and can experience eczema flare-ups. Areas of inflamed skin can become red or darker, depending on a child’s skin tone, and be very itchy and sore. The itch can, at times, became almost unbearable, causing a child to want to scratch constantly, especially at night, thereby interfering with sleep. If a child has moderate to severe atopic eczema, they may scratch until their skin bleeds. However, since the skin is very dry, it can also crack and bleed of its own accord. Any cracked, raw or bleeding areas are especially vulnerable to infection.

Atopic eczema usually appears during the first few months of life, often starting on the face and scalp. It can be present on any area of the body. In light- skinned children it usually affects the skin creases, neck, back of knees and inside of elbows. There may also be roundish, dime sized-shaped areas of eczema, known as ‘discoid eczema’.

Children of colour often have different patterns of eczema. These include eczema around the front of the knees and the back of the elbows as well as in the creases, as seen on white skin. Fine bumps over the chest and tummy, are also common.
If the eczema has been persistent, the skin may feel and look thickened in areas where there has been lots of rubbing and scratching. Atopic eczema can vary in severity between different children. Some children have dry skin and eczema that can be kept under control with simple treatments, while others may need a variety of more complex treatments. You will get to know what your child’s eczema looks like, what treatments will be needed for flares (when the skin becomes hot, inflamed, itchy and sore) and when your child needs to visit a healthcare professional. However, if the eczema gets worse (becomes difficult to control, or wet and weepy with yellow crusts, or spreads rapidly to other parts of the body), you should always ask for medical help. This may indicate severe infection, which would need prompt treatment.
Is there a cure for eczema?
Unfortunately, at present there isn’t, but it can usually be well managed, allowing the majority of children to lead a normal life. The nature of eczema is a cycle of controlled eczema (but dry skin is a constant) and inflamed skin ‘flares’.
Why does my child have eczema?
Hereditary factors seem to play a role in the development of childhood There is often a family history of eczema, asthma or hay fever. If one or both parents have eczema, asthma or hay fever, the risk of their children developing eczema increases. A child can develop one or more of these conditions and does not always develop the same one/s as their parents. There are also many environmental factors that may play a role. These often include climate, temperature, house dust mites and pollen, as well as individual triggers.

What are the most common triggers and how can I avoid them?

Triggers are environmental factors (they may be irritants or allergens) that cause a child’s eczema to worsen or ‘flare’. These vary from individual to individual and it can be difficult to identify them as they might not trigger an immediate or noticeable reaction. Some of the most common triggers are:
Soap and water – Avoid washing in plain water and using soap or bubble bath. These damage the skin barrier, causing more dryness and irritation.
Fragrance – Avoid fragranced (perfumed) products. Bear in mind that perfume can act as an airborne allergen.
Temperature – Being too hot or too cold or going from one temperature to another can trigger a bout of itching. Many children with eczema get hot quickly, so dressing in thin layers can help.
Sweat – Aside from avoiding becoming hot and sticky, cotton clothing can be helpful.
Wet and messy play – e.g. sand, water, paint, clay. Hands should be moisturised before these kinds of activities, then washed with a soap substitute and moisturised with emollients) afterwards. PVC gloves with a cotton glove liner can help.
Clothing – Wool and synthetic materials can be particularly uncomfortable. 100% cotton, garments worn under abrasive materials are best. Avoid garments with seams or labels that can chafe, or cut labels out.
House dust mites – House dust mites are present in all homes and it is impossible to eradicate them. They thrive in warm, moist environments, particularly mattresses. House dust mite droppings can exacerbate eczema and 80% of children with eczema skin prick test positive to them, so may be allergic to them. Washing clothing and bedding at 60°C kills them.
Animals – If you have pets, make sure they are kept away from your child’s bedroom. Animal dander, saliva and fur can all be irritants, so make sure you clean rooms regularly and that your child washes their hands after stroking or handling animals.
Food – A few children with eczema have food allergies, the most common being egg, nuts, sesame and cow’s milk. Generally a food allergy is identified before a child is 2 years old. It is important for children to have a good, balanced diet. Children can also have an irritant reaction on their face to food, but this is not an allergy.
Damp and mould – Spores from rotting vegetation and mould in buildings can make some children’s eczema worse.
Swimming pools – Chlorine and other chemicals added to swimming pool water can have an adverse effect on the skin, so always apply a protective layer of emollient 30 minutes to 1 hour before into the pool. After the swim, if the pool showers use chlorinated pool water, it may be best to go home and take a shower there. Reapply emollient after the shower.
My child has a problem with light and dark patches of skin due to his eczema. Why is this?

Some children with eczema develop round or oval pale patches that appear when a flare has settled. This is a normal symptom of eczema called pityriasis alba. It affects children of all ethnicities, but can be more noticeable in children with darker skin tones. It is also more prominent after being in the sun because of the effect of tanning of non-affected skin. Colour should gradually return to normal, but the patches can persist for 2–3 years. In children of colour, the areas of skin affected by eczema can become lighter or darker. This is because of changes in skin pigmentation caused by eczema inflammation. The dark patches are usually active areas of eczema, which may also be red. The lighter patches often occur when your child’s eczema is clearing (and may also be pityriasis alba) These pigment changes may be seen on the skin for several months as they take a long time to settle down. Eventually normal skin pigment should return.
Will my child grow out of eczema?
Eczema improves for most children as they get older – about two-thirds are clear by puberty – but they will always have sensitive skin, and the eczema may return. Some children continue to have problematic eczema throughout life while others may find that their eczema goes away sometime during their childhood, only to come back in adulthood. There is no way we can predict the natural course of your child’s eczema – the important thing is to take and keep control of it.
In our next blog post, we shall discuss treatments in detail.