Treating Eczema
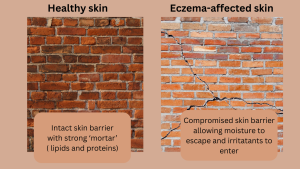
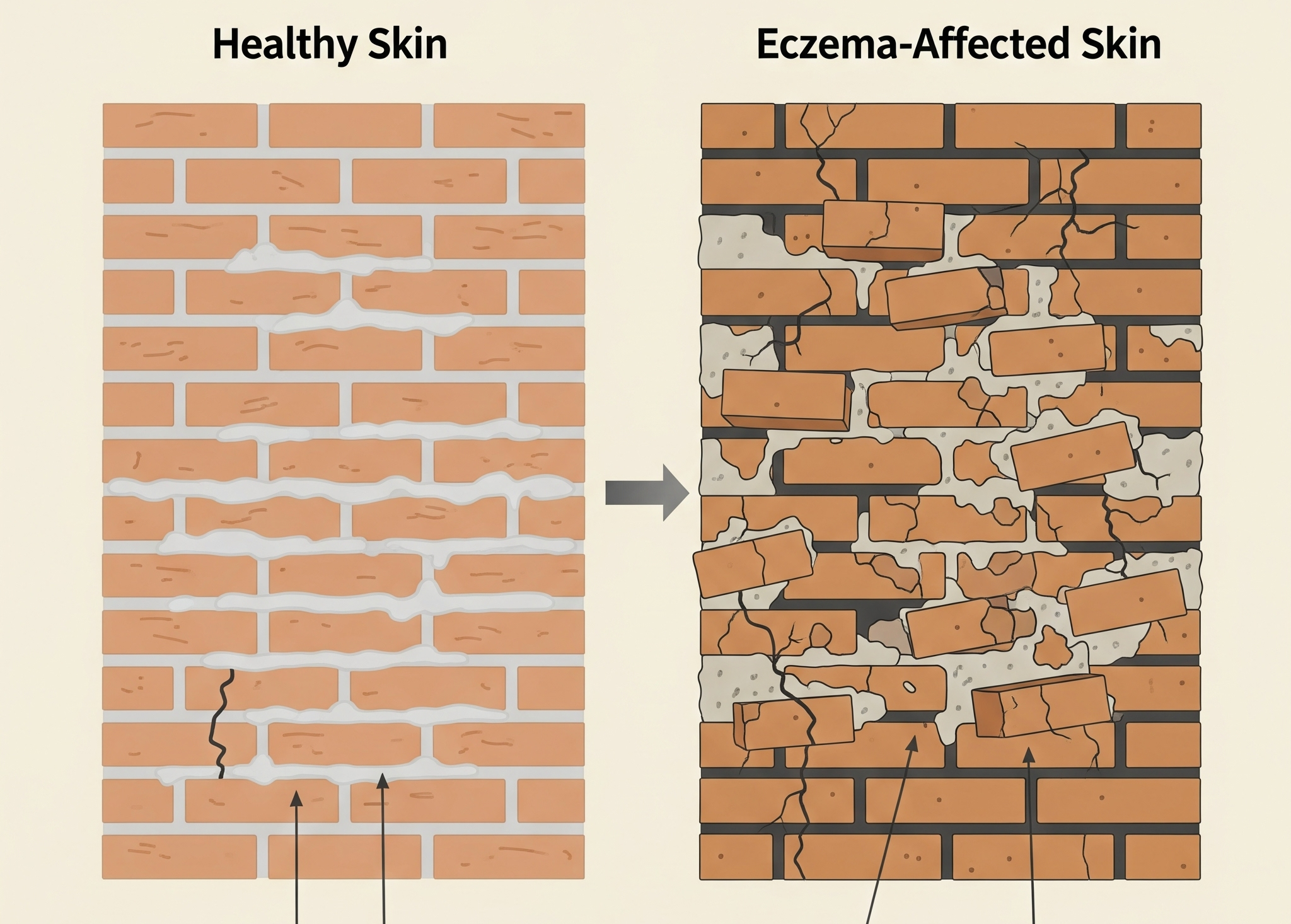
Children with atopic eczema have dry skin. A simple way to understand this is to think of skin as a brick wall.
Healthy Skin as a Solid Wall
- Bricks: The individual skin cells are like the bricks.
- Mortar: The natural fats and oils (lipids), such as ceramides, cholesterol, and fatty acids, that fill the spaces between the cells are the mortar.
In healthy skin, this “wall” is strong and intact. The lipids act as a protective seal, keeping essential moisture locked inside and preventing allergens, irritants, and bacteria from getting in.
Eczema Skin as a Damaged Wall
In a person with eczema, this wall is compromised.
- Broken Mortar: Due to genetic factors, like a mutation in the filaggrin protein, the skin doesn’t produce enough of the natural fats and oils. This leads to a weak, crumbling mortar with gaps and cracks.
- Leaky Wall: With the mortar failing, the wall can’t hold moisture. This leads to transepidermal water loss, making the skin dry, flaky, and itchy.
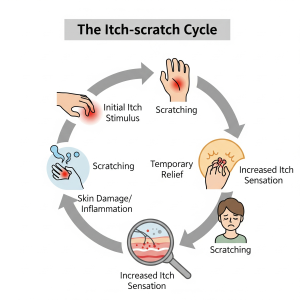
- Vulnerable to Invaders: The cracks in the wall allow external irritants, allergens, and bacteria to easily penetrate the skin. This triggers an immune response, leading to inflammation, redness, and the classic itch-scratch cycle of eczema.
This analogy helps to explain why moisturizing is the cornerstone of eczema management— it’s like applying new “mortar” to the damaged wall to restore its protective function. You must use emollients every day even when the skin looks good, as this will help prevent further ‘flare-ups’ of eczema and help to keep the important skin barrier intact. Emollients are medical moisturisers which come as ointments, creams, lotions, and gels to be left on the skin, and as washes and bath oils/shower gels to be used as soap substitutes.

Which emollient should I use?
Emollients come in the form of ointments, creams, lotions, and gels. These can be left on the skin and are known as leave-on emollients (most can also be used as soap substitutes). There are also emollient bath/shower washes, which are used for washing and are rinsed off.
You should apply leave-on emollient every 3–4 hours if possible, depending on the type being used (e.g. ointment, cream or lotion) and the dryness of your child’s skin. Creams, lotions and gels need to be applied more frequently than ointments, although emollients containing humectant ingredients may need to be applied less frequently, as their moisturising effects last longer. Soap substitutes (which may be emollient wash products or leave-on emollient used as a soap substitute).
Types of emollients
Ointments are the greasiest type of emollient. They contain fewer preservatives than other emollients and do not require stabilising additives, which creams, gels and lotions do. (Preservatives and stabilising ingredients can cause an irritant or allergic reaction in some children). They can give a good seal on the skin and are excellent at restoring barrier function to the skin. They do make clothes oily, but they are a good choice for bedtime and when not wearing special clothes.
Creams are lighter and absorbed more quickly into the skin.Understandably, many parents prefer to be prescribed a cream. Gels are similar in consistency to creams.
Lotions are the lightest type of emollient. They are good for areas of infected eczema or for very hairy areas, such as scalps or under the arms.
If your child has moderate to severe eczema, the solution may be to use a cream during the day and an ointment at night. Some emollients contain added ingredients, such as the humectants urea or glycerol (natural moisturising factors), anti-itch and anti-bacterial additives. Creams and lotions must also contain preservatives and stabilising additives (to keep the oil and water mixed), which in a few children can cause an allergic or irritant reaction, but preservatives are all essential for product safety and preventing contamination.
Most emollients are available on prescription for children and can also be bought from chemists. A doctor should be able to advise you. The key is to find those which suit your child, and this can only be done by trial and error. It is quite possible that you will find that a combination works best – for example, a greasier ointment where the skin is very dry, and a cream or lotion if the eczema is a bit weepy. Try to use any new emollient for at least a month unless you can see it is making the eczema worse. It is a good idea to patch test a new product on a small area of eczema-free skin every day for 5 days and check for signs of an allergic or irritant reaction. If the skin reacts, stop using the product.
How do I apply the leave-on emollient?
Apply large ‘blobs’ of the emollient on to the skin generously a few centimetres apart and then smooth it in, using gentle downward strokes in the direction of hair growth. Never rub it in, as thick emollients sometimes block the hair follicles in the skin, which may cause a mild inflammation or infection of the affected hair follicles. There is good evidence that less topical steroid may be needed if the skin is regularly moisturised. If you use pots, decant the cream or ointment with a spoon before application to avoid contaminating the product with your fingers. If using creams, a good alternative is pump dispensers.
Children with eczema need to be prescribed large quantities of emollient at a time – a child with atopic eczema will need to use about 250g of emollient per week (or up to 500g per week for a bigger child), and more if the eczema is severe. When you find an emollient that your child likes and that suits their skin, ask for it to be on repeat prescription and in large amounts (e.g. a 500g pump or tub and a 200ml bottle for wash products) so you never run out. Small dispensers or tubs are also useful for taking to school and when you are out and about.
Why Soap Substitutes?
Ordinary soap and bubble baths degrease the skin and damage the skin barrier, leading to drying out of the skin. Soap substitutes are used with water and will clean the skin just as well as soap in most circumstances. A soap substitute may be an emollient wash product or your child’s regular leave-on emollient. To use leave-on emollient as a soap substitute, simply apply it to your child’s skin and then rinse it off. Bath oils can also help cleanse the skin. You should not wash your child with water alone, as water can be very drying.

What about bathing?
Daily bathing is considered optimal for most children with eczema. Bathing should be for less than 10 minutes, as after this time the skin becomes more fragile and subsequent scratching will cause more damage. The bath water should be warm but not hot – if the water is too hot this may trigger itching. Never use bubble bath as it can be very drying and irritating to some skins. Instead, apply your child’s emollient all over their body before they get into the bath and then simply let them soak and rinse off in the bath. As an alternative to bath oil, add a tablespoon of emollient to the bath as you fill it. The oil and water mix will clean the skin as well as coat it with a film of oil which traps water and prevents the skin drying out. Emollients can make the bath slippery, so be sure to use a bath mat and clean baths and showers daily to prevent accidents and the build-up of grease. White vinegar is a good cleaning product for the bath. After bathing, pat the skin dry with a soft towel and reapply the leave-on emollient.
Can my child shower instead of bathing? Generally, bathing is recommended, as immersing in an emollient bath is a good way to help moisturise and cleanse the skin. If you do not have a bath or prefer other methods of washing, it is acceptable to apply emollients and then rinse them off using a shower or a bucket of water and a cup, for example. Younger children may also be ‘bucket bathed and rinsed’. Water used for showering and rinsing should be warm but not hot. Ordinary shower gels should be avoided as they can be very drying and irritating to some skins; instead, use emollient shower or wash products or a leave-on emollient as a soap substitute – but take care as they can make the shower floor very slippery.
After washing or showering, pat the skin dry with a soft towel and reapply the leave-on emollient.

What are Topical Steroids and are They Safe?
Topical steroids are recommendedfor treating eczema flare-ups and have been used for several decades. Topical’ means applied directly to the skin. ‘Steroids’ are a group of natural hormones, produced in the body by a variety of different glands. They are also produced synthetically as medicines.
Topical steroids act on the skin to reduce inflammation and itch, and speed up healing. Topical steroids generally come in four different strengths (mild, moderate, potent and very potent) – for example, hydrocortisone is mild, mometasone is potent and clobetasol is very potent (check the patient information leaflet or ask the pharmacist if you are not sure). The chances of any side effects occurring increase with the strength of the steroid. Topical steroids should be used for short-term flare treatment only. Doctors may advise using them for 2 weeks: once a day for 7 days and then once every other day for a further 7 days. Sometimes, if the eczema is more severe or still flaring, continued ‘weekend therapy’ is recommended. Weekend therapy means applying topical steroid on 2 consecutive days each week, usually for no more than a couple of months. Topical steroids are effective treatments for eczema, but like many medicines, they can have side effects including thinning of the skin. When used for short treatment bursts as directed by a healthcare professional, and applied to areas of affected skin only, the risk of side effects is small.
Some people are concerned about possible side effects when their child stops using topical steroids (namely ‘topical steroid withdrawal’, TSW). Baby and child eczema often comes back after a topical steroid is stopped, but this is unlikely to be TSW. If it flares up immediately on stopping, this usually means that the eczema is still active and still needs active treatment to control it.
Eczema is complex and has significant effects on both physical and psychological wellbeing. It must be treated effectively to control itch and inflammation, to minimise scratching with its risk of permanent scarring, and to re-establish the skin barrier.
How do I apply the topical steroid?
Topical steroids should be applied as instructed. This will usually be once or twice a day, only to the areas of inflammation (i.e. the areas of active eczema). Apply as a thin layer and in smooth, downward strokes. The surface of the skin should ‘glisten’ once the steroid has been applied. Another method of applying topical steroids isthe fingertip unit (FTU) application.

How much topical steroid do I need to use?
There are guidelines on the amount of topical steroid required to cover different body areas affected by eczema. These are based on the Finger Tip Unit (FTU), which is the amount of cream or ointment that covers the end of an adult finger (tip to skin crease). One FTU is enough to cover an area of skin the size of one adult hand.
Studies have shown that it is more effective to apply a topical steroid before an emollient. It is important that you leave a gap -about 20 minutes- between the steroid and emollient.
Topical calcineurin inhibitors
These include pimecrolimus cream and tacrolimus ointment. They are prescribed for children and adults as an alternative to topical steroids, especially when the eczema is not being adequately controlled by topical steroids or is located on areas of thebody where the skin is very delicate, such as the face, neck and groin.TCIs are usually applied twice a day for short periods to treat flares, or twice a week on non-consecutive days as maintenance treatment. Pimecrolimus can be prescribed for children aged 3 months of age and older, and tacrolimus for children aged 2 years and older (but may be prescribed by a dermatologist “off-license” for younger kids).
Do antihistamines help?
Antihistamines do not actually treat the itch, as eczema is not caused by histamine. Sedating antihistamines may be prescribed to help your child sleep at night. Sedating antihistamines are meant to be used for a short time when the eczema has flared up, and not as a long-term measure. Antihistamines should be given to the child at least half an hour before bedtime, so that they are not sleepy in the morning.
Antihistamine creams are not effective for treating eczema.